**If you answered yes to any of these questions talk to a healthcare provider or your physician. You may benefit from pelvic floor PT. Got questions? Let's talk...
Click Here to Schedule a Free 20 Minute Phone Call with Gia PT
Click on the button for a free Bladder Diary - it is also called a Bladder Voiding Log. Fill out this log for 5 days and bring them with you to your 1st visit.
Click here for Bladder Log
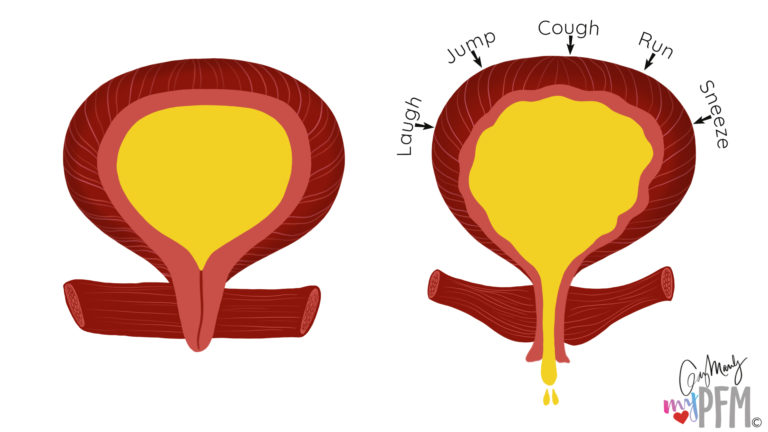
Incontinence effects millions of people in the United States. At Gia McDaniel Physical Therapy we help women with a variety of types of urinary/fecal incontinence. Often we have an issue with the contractility or relaxation capabilities of the pelvic floor musculature. Treatment is focused at understanding your symptoms and in designing a treatment strategy to improve the quality of your life. Types of incontinence include Stress Urinary Incontinence (SUI), Urge Incontinence, Urinary frequency/OAB, Neurogenic Incontinence and Fecal Incontinence.
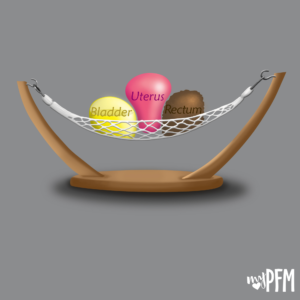
Stress Urinary Incontinence: This can often arise in patients that have a weakened support structure whether in their inherent tissue or acquired after pelvic floor trauma, surgery, or uncontrolled trunk pressures.
Inherent tissue problems may lie in the substance of the patient’s own connective tissue. There may be excessive laxity in the fascial coverings around the lower pelvic organs. This may lead to further issues down the road that may contribute to the development of a prolapse, cystocele, or rectocele.
Connective tissue laxity problems; however, can also be something that occurs and increases over many years. For example if you have chronic cough – that sharp increase in abdominal pressure that presses on the pelvic organs and occurs over a long period of time – may also contribute to a laxity problem in you trunk or pelvic support structures.
Post Partum women often have a predisposition for both poor contractility and increased laxity in pelvic tissues because of the trauma the pelvic tissues have experienced related to child birth.
Urge Incontinence/Urinary Frequency: Both of these conditions may involve brain awareness training. Continence is associated with learned behavior . The brain’s response is also a component of bladder retraining techniques. Bladder responses involve behavioral modifications. It is these behavioral modifications that offer a window into affecting the brain’s ability to modulate it’s response and hopefully improve continence. For example, what emotional connections with your toileting habits? Do you always got the bathroom before you leave the house because that is your routine? Sometimes this can be a learned bladder routine from childhood that has been integrated into our adult life.
Neurogenic Bladder: These are issues related to problems with the communication between the bladder and the brain. This may be experienced by persons with Parkinson’s Disease, Multiple Sclerosis, CVA, or traumatic brain injury. A neurologist will likely offer guidance to the patient with bladder dysfunction due to neuorgenic causes. Sometimes patients with neurogenic dysfunction do benefit from physical therapy to enhance recruitment and awareness of their pelvic floor muscles and other overflow muscles. This can be further discussed with your therapist.
Interested in learning more? Would you like to tell me about what you are experiencing and see if you are a good candidate for continence rehabilitation services?